Living with oesophageal cancer
A diagnosis of oesophageal cancer can affect many parts of your life, not just your body. It can change how you eat, how much energy you have, how you feel emotionally, and how you manage day-to-day tasks.
Living well means learning to manage symptoms and treatment side effects, adjusting to changes in eating and swallowing, taking care of your mental health, and getting the right support when you need it.
This section offers practical tips and guidance to help you handle everyday life with oesophageal cancer – from caring for your body to looking after your mind.
Managing symptoms and side effects
Because oesophageal cancer affects your digestive system, eating and drinking can become challenging. The side effects of treatment can make things even harder.
Some days will feel more difficult than others. Understanding what's happening and learning how to manage your symptoms and side effects can make a big difference in how you feel.
Most of these symptoms can be managed with the right care and support. Your healthcare team is there to help with these issues. They're all a normal part of living with oesophageal cancer and its treatment.

Common symptoms and side effects
Treatment for oesophageal cancer can cause a range of side effects. You might experience all, some, or none of these. Everyone's experience is different.
Common side effects include:
- difficulty swallowing (dysphagia) or painful swallowing
- feeling of food getting stuck or choking when swallowing
- reflux and heartburn
- nausea and vomiting
- loss of appetite and feeling full quickly
- changes in taste or smell
- mouth dryness or throat soreness
- fatigue
- weight loss
- diarrhoea or constipation
- pain.
If you're experiencing any of these symptoms, talk to your healthcare team. There are ways to manage most of them.
Difficulty swallowing (dysphagia)
Difficulty swallowing is one of the most common challenges after oesophageal surgery or radiotherapy. This happens because of changes to your oesophagus, which can be caused by the tumour location or as a side effect from treatment.
You may also cough while eating or feel as though food is 'going down the wrong way'. If you're coughing or spluttering when eating or drinking, you should see your doctor right away, as these problems can be serious.
Tips to make swallowing easier:
- Chop, mince or puree food to make smaller pieces that are easier to swallow
- Snack on soft foods between meals, such as avocado, yoghurt, custard, ice cream, diced tinned fruit and milkshakes
- Try eating soft, nutritious foods, such as scrambled eggs, porridge, soup and casseroles
- Make tough food softer by using a slow cooker to keep food soft and moist, mash your food with a fork, or add extra gravy or sauce to your meals
- Sit upright and chew carefully and slowly. Avoid lying down within 30 minutes of eating or drinking
- Wash food down with small sips of a drink
- Make changes in texture of food and thickening of fluids as guided by your dietitian and speech pathologist.
Your dietitian and speech pathologist can work with you to find the best approach for your swallowing difficulties.
Reflux and heartburn
Reflux and heartburn are common after oesophageal surgery or radiotherapy. They occur when stomach acid flows back up into your oesophagus.
Tips to manage reflux:
- Eat small, frequent meals instead of three large meals
- Avoid foods and drinks that trigger your reflux, such as fatty or spicy foods, citrus, tomato-based foods, chocolate, and coffee
- Don't lie down within 2-3 hours after eating
- Sleep with your upper body elevated (raise the head of your bed or use extra pillows)
- Avoid tight clothing around your waist
- Talk to your doctor about medications that can help reduce acid.
Nausea and vomiting
Nausea and vomiting can be caused by the cancer itself, or by treatments like chemotherapy and radiotherapy.
Tips to manage nausea:
- Eat small, frequent meals throughout the day rather than three large meals
- Stick to bland, easy-to-digest foods like crackers, toast, rice, bananas, and plain pasta
- Avoid fatty, fried, or very sweet foods
- Eat cold or room-temperature foods, which may be easier to tolerate than hot foods
- Sip fluids slowly throughout the day to stay hydrated
- Rest after eating, but keep your head elevated
- Try ginger tea or ginger lollies, which can help settle your stomach.
Your doctor can prescribe anti-nausea medications that can help. Don't wait until symptoms become severe - talk to your healthcare team as soon as you feel unwell.
Fatigue
Fatigue is one of the most common side effects of cancer and its treatment. It's more than just feeling tired - it's an overwhelming exhaustion that doesn't get better with rest.
Tips to manage fatigue:
- Balance activity with rest. Plan activities for times when you have more energy
- Take short naps (20-30 minutes) during the day if needed, but avoid long daytime sleeps
- Stay as physically active as you can. Even gentle activities like short walks can help boost energy
- Ask for help with daily tasks when you need it
- Eat well and stay hydrated
- Talk to your doctor if fatigue is affecting your quality of life - there may be underlying causes that can be treated.
Loss of appetite and feeling full quickly
It's common to lose your appetite or feel full after eating only small amounts. This can be due to the cancer, treatment, or changes to your digestive system.
Tips to manage poor appetite:
- Eat small amounts more frequently throughout the day - aim for 5-6 small meals instead of 3 large ones
- Keep nutritious snacks handy, like nuts, cheese, yoghurt, or smoothies
- Make every bite count by choosing foods that are high in protein and energy
- Drink nutritious fluids like milk, milkshakes, smoothies, or soup
- Try to eat at times when you feel most hungry, even if it's not a traditional mealtime
- Make mealtimes pleasant - eat with others when you can, and in a comfortable environment.
A dietitian can help you plan meals and suggest ways to boost your nutrition, even when you don't feel like eating.
Changes in taste or smell
Chemotherapy and radiotherapy can affect how food tastes and smells. Some people find that foods taste metallic, bland, or just different from usual.
Tips to manage taste changes:
- Experiment with different foods to find what tastes good to you now
- If red meat tastes strange, try other protein sources like chicken, fish, eggs, cheese, beans, or tofu
- Use plastic utensils if you're experiencing a metallic taste
- Add flavour with herbs, spices, marinades, or sauces
- Rinse your mouth before meals
- Try cold or room-temperature foods if hot foods taste strange
- Keep your mouth clean by brushing your teeth regularly.
Most taste changes improve after treatment ends, though it may take several weeks or months.
Mouth dryness and throat soreness
Radiotherapy to the chest area can cause mouth dryness and throat soreness.
Tips to manage mouth and throat problems:
- Sip water frequently throughout the day
- Suck on ice chips or ice blocks
- Use a humidifier in your bedroom at night
- Avoid alcohol, caffeine, and tobacco, which can make dryness worse
- Choose soft, moist foods
- Rinse your mouth regularly with water or a mild salt water rinse
- Talk to your doctor about artificial saliva products or medications that can help increase saliva production
- Keep your lips moist with lip balm.
Changes in bowel habits
Treatment can affect your bowel movements, causing diarrhoea or constipation.
For diarrhoea:
- Drink plenty of fluids to replace what you're losing
- Eat small, frequent meals
- Choose low-fibre foods like white rice, white bread, bananas, and plain pasta
- Avoid fatty, fried, or very sweet foods
- Limit caffeine, alcohol, and dairy if they make symptoms worse
- Talk to your doctor about medications that can help.
For constipation:
- Drink plenty of fluids
- Eat high-fibre foods if your doctor agrees this is suitable for you
- Stay as physically active as you can
- Talk to your doctor about stool softeners or laxatives if needed.
Pain
If pain is your main issue, you may be referred to a pain specialist to help manage it.
Your GP should be sent a letter explaining your condition, and you should be given the name of a person at the hospital to contact if you have any concerns or need additional support.
Types of pain management include:
- Medications (your doctor can prescribe different types of pain relief)
- Heat packs or cold packs
- Gentle massage
- Relaxation techniques
- Physiotherapy.
You should never have to live with unmanaged pain. Your healthcare team can work with you to find the right combination of treatments to keep you comfortable.
When to see help
Contact your healthcare team immediately if you experience:
- severe or worsening pain
- persistent vomiting that stops you from eating or drinking
- signs of dehydration (dark urine, dizziness, extreme thirst)
- fever or signs of infection
- significant weight loss
- complete inability to swallow food or fluids
- coughing or choking when eating or drinking
- blood in your vomit or black, tarry stools
- any new or worsening symptoms that concern you.
These symptoms might indicate complications requiring prompt medical attention.
Your emotional and mental health
A diagnosis of oesophageal cancer can affect you emotionally as well as physically. It's normal to experience a wide range of feelings, and these feelings may change from day to day.
Looking after your emotional and mental health is just as important as managing physical symptoms. Taking time to understand your feelings and finding ways to cope can make a real difference to your quality of life.
Your emotions
Everyone reacts differently to a cancer diagnosis, but some common feelings include:
- shock and disbelief, especially when first diagnosed
- fear and anxiety about treatment, the future, or cancer coming back
- angry at the unfairness of the situation
- sad about changes to your life and future
- guilty about being a burden on others or about past lifestyle choices
- a loss of control, like cancer is controlling your life
- hope when treatment goes well or you have good days
- gratitude for support from loved ones and healthcare teams.
You might experience all of these feelings, some of them, or different emotions entirely. There's no right or wrong way to feel.
Over time, you may go through a range of emotions, from feeling positive and determined to beat the cancer to feeling low or despairing about the future. This is normal.

Ways to support your emotional wellbeing
There are many strategies than can help you manage the emotional impact of living with oesophageal cancer. What works for someone else may not always work for you. It is important to keep this in mind during your treatment.
- Talk about your feelings. Keeping feelings bottled up typically intensifies distress. Share with trusted friends or family, join a support group where others truly understand, or talk with a counsellor via the Pancare Support Helpline. Saying difficult things aloud often lessens their power.
- Keep some routines. Cancer can turn life upside down, but holding onto small routines, like going to bed and waking up at the same time, can bring a sense of calm and control.
- Be kind to yourself. You’re going through something really difficult. Treat yourself the way you would treat a friend, with patience and compassion. Rest when you need to, let yourself cry, and celebrate small wins.
- Take breaks from cancer information. It’s natural to want to learn about your illness, but constantly reading online or searching for statistics can make anxiety worse. Try setting limits on how much time you spend researching.
- Find small moments of joy. Even on hard days, small pleasures can lift your spirits. Try watching a funny movie, listening to music, sitting in the sun, or cuddling a pet. These little things matter.
- Try relaxation or mindfulness. Deep breathing, gentle stretching, meditation or guided imagery can help ease stress and improve sleep. Many hospitals offer relaxation classes, or you can try free apps at home.
- Stay connected. When you don’t feel social, it’s easy to pull away. But staying in touch helps. A short visit, text, or video chat can remind you that you’re supported and not alone.
- Move your body when you can. Even a slow walk or some gentle stretching can boost your mood and energy. Movement helps both your body and mind feel stronger.
When feelings become overwhelming
While it's normal to feel anxious, sad, or worried, sometimes these feelings can become overwhelming. You might need extra support if you're feeling very anxious or worried most of the time.
Signs that you might need extra help from your healthcare team include:
- difficulty sleeping or sleeping too much
- loss of interest in things you usually enjoy
- difficulty concentrating or making decisions
- withdrawing from family and friends
- feeling hopeless about the future
- having physical symptoms like a racing heart, difficulty breathing, or panic attacks
- having thoughts of self-harm all mean you should reach out for help.
If you're experiencing any of these, please talk to your healthcare team, GP, or a counsellor. Help is available, and you don't have to cope alone.

Fear of cancer returning
After finishing initial treatment for oesophageal cancer, many people worry about the cancer coming back. This is a normal fear.
It’s important to focus on follow-up care and the things you can control rather than what you can't.
Talking about your worries can help and connecting with others who understand these fears can be reassuring.
If this fear is affecting your daily life, talk with your healthcare team.
Diet and nutrition
Good nutrition is one of the most important things you can do to support your body through oesophageal cancer and its treatment.
Because oesophageal cancer affects your digestive system, eating and drinking can become challenging. Managing these changes is important for your recovery, and will make you feel better in general.
Working with a dietitian who understands oesophageal cancer can make a big difference. They can help you plan meals that work for your body's new needs and manage symptoms.

Why nutrition matters
Oesophageal cancer and its treatment can place extra demands on your body, greatly increasing your nutrient and energy needs, which can lead to weight loss.
Weight loss can contribute to fatigue, delay and lengthen recovery, and negatively affect your quality of life. Because the cancer affects the digestive system, you might find it even more difficult to get enough nutrition to meet your needs and maintain weight.
Good nutrition can help you:
- Maintain your strength and energy
- Support your immune system
- Help your body recover from treatment
- Manage side effects better
- Improve your quality of life.
Eating after oesophageal surgery
After your surgery, what and how you can eat will depend on the type of operation you’ve had and what your hospital team recommends.
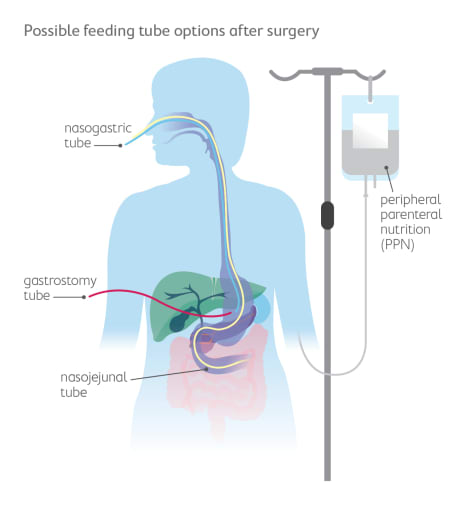
Sometimes it’s hard to get enough food and energy by eating normally. Your doctor or dietitian might suggest using a feeding tube to help your body get the nutrition it needs to heal.
- A feeding tube can go directly into your stomach or small intestine before surgery (called a gastrostomy or jejunostomy).
- Sometimes a soft tube is placed through your nose and down into your stomach (called a nasogastric or nasojejunal tube) during or after surgery if eating is difficult.
These tubes help your body get the right nutrients while your oesophagus and stomach are healing. A special liquid food (called a feeding formula) is given through the tube until you’re ready to eat and drink again.
When you start eating, you’ll begin with liquid or smooth foods like soups or pureed meals. Then you can slowly move to soft foods for a few weeks. Your surgeon or dietitian will tell you when it’s safe to eat solid foods again.
They may also suggest eating small meals or snacks often instead of a few big meals. The hospital dietitian can help make a meal plan and recommend any supplements to help you get enough energy and nutrients.
Common eating challenges
Treatment can cause tiredness, changes in taste or smell, mouth or throat soreness, reflux, nausea, or problems swallowing. These symptoms can make eating difficult, but there are ways to help:
- Eat soft, moist foods like soups, casseroles, or smoothies.
- Sip nourishing fluids such as milk, smoothies, or soups between meals.
- Try cold foods if smells bother you.
- Add sauces or gravies to keep food moist.
- Sit upright while eating and for at least 30 minutes afterwards.
Managing weight and energy
Some people lose weight during treatment, while others gain weight. Both can be normal.
If you’re losing weight or feel weak, focus on high-energy, high-protein foods such as:
- Meat, fish, eggs, dairy, legumes, nuts, and seeds.
- Cream, avocado, butter, nut butters, and oils.
- Fortifying foods—like adding milk powder to milk or blending nut butter into smoothies—helps you get more energy without eating extra food.
If you gain weight, a dietitian can help you make small, healthy changes to balance your meals.
Building a healthy diet
A healthy diet gives your body energy to recover and helps wounds heal.
- Eat a variety of foods from all food groups.
- Try six small meals or snacks each day.
- Eat the most nourishing foods first if you fill up quickly.
- Make the most of the times you feel hungry.
Smoothies and milkshakes are easy ways to add energy and protein when your appetite is low.
Working with a dietitian
A dietitian who understands oesophageal cancer can make a big difference. They can help you:
- understand your body’s new needs
- plan meals that fit your lifestyle
- manage symptoms like dumping, reflux, or feeling full quickly
- prevent nutrition problems before they start.
Ask your healthcare team for a referral to a dietitian. This is one of the most important things you can do to help yourself feel better.
Living well with oesophageal cancer
Oesophageal cancer doesn't have to stop you from living a meaningful and full life.
While acknowledging the challenges, finding ways to stay active, maintain relationships, and engage in activities that bring satisfaction helps you feel more like yourself and improves both physical and emotional wellbeing.
Living well doesn't mean pretending everything is fine or maintaining your pre-cancer pace. It means identifying what matters most to you now and finding adapted ways to pursue those things.
Physical activity and exercise
When you’re dealing with oesophageal cancer and its treatments, exercise might feel impossible or unimportant. But gentle movement can actually help you feel better.
Research shows that the right kind of activity can:
- boost your energy and reduce tiredness
- help keep your muscles strong
- lift your mood and improve sleep
- support digestion and appetite
- even help your body respond better to treatment.
This isn’t about hard workouts or gym goals. It’s about moving in ways that feel right for you.
After surgery, start small and take your time. Walking is one of the best choices. Even short walks of a few minutes at a time can help your body heal and regain strength.
During chemotherapy, your energy may change from day to day. On good days, you might walk a little further or do light exercise. On tired days, even gentle stretching or a slow lap around the house counts. The goal is to move your body most days, not to push yourself too hard.
Ideas for gentle activities
- Walking outdoors or inside (like at a shopping centre)
- Swimming or water exercises (once your surgical wounds are fully healed)
- Gentle yoga or tai chi for balance and flexibility
- Using light weights or stretchy bands to keep muscles strong
- Stationary cycling
- Gardening or dancing
- Playing with children or grandchildren
Working with professionals
An exercise physiologist or physiotherapist who understands cancer care can help you build a safe and effective plan. They can adjust your program as your condition changes to make sure you’re exercising safely and getting the most benefit.
You can ask your healthcare team for a referral to an exercise professional.
Relationships
Oesophageal cancer can affect your relationships in many ways. Physical changes, tiredness, stress, treatment, and changes in eating can all affect how you connect with your partner, family, and friends.
Talking to loved ones
Share how you’re feeling and let people know how they can help. You don’t need to protect others by hiding your emotions. It’s okay to talk about everyday things. Not every conversation has to be about cancer.

When relationships feel strained
People who care about you often want to help but may not know how. Some might hover too closely, while others stay away because they feel unsure. The best way to help them support you is to talk openly and clearly about what you need.
You might say things like:
- “I’d love help with grocery shopping on Thursdays.”
- “Can we talk about something other than cancer for a bit?”
- “Just sitting together without talking really helps.”
Intimacy and sexuality
Cancer and its treatments can affect your interest in sex and physical closeness. You might feel too tired, sore, or anxious. Changes in your body, such as scars or weight loss, can also make you feel self-conscious. These are very common feelings, and they do not mean something is wrong with you.
Tips that may help
- Talk honestly with your partner about what feels okay and what doesn’t
- Remember that intimacy isn’t only about sex. Touch, hugs, and closeness can be just as important
- Choose times when you feel rested or less unwell
- Speak with your doctor if pain, nausea, or other side effects make intimacy hard
- A counsellor or sex therapist can help if these changes cause stress in your relationship
Intimacy needs change over time. Be kind to yourself and keep communication open.
Staying social when eating is hard
Because food is a big part of most social events, eating differently can make gatherings feel awkward. But staying connected is important for your wellbeing.
Try these ideas:
- Meet friends for activities that don’t revolve around food, like going for a walk, to a park, movie, or gallery.
- If you’re meeting for a meal, eat a little beforehand and focus on the company, not the food.
- Host get-togethers at home where you can plan the food and timing.
- Let close friends know your situation in a simple way so they understand and don’t worry.
- Pick restaurants where you know there’s something small or soft you can eat.
Remember: your friends and family care about you, not what or how much you eat. Staying connected helps you feel supported and less alone.
Finding meaning and purpose
Many people find comfort in spending time on things that matter most – whether that’s hobbies, family, faith, creativity, or being in nature.
You might enjoy gentle yoga, meditation, music or art therapy, reading, gardening, or spiritual activities.
Small moments of joy can make a big difference.
Practical support during oesophageal cancer
An oesophageal cancer diagnosis brings practical challenges alongside medical ones. Managing work, finances, and daily tasks can feel overwhelming when you're also dealing with treatment and recovery.
Getting the right practical support can reduce stress and allow you to focus on your health. You don't have to manage everything alone.
Work and employment
Your diagnosis will affect your ability to work, even if it is only temporarily such as when having treatment.
It's important to talk to your employer about your diagnosis and likely time off work, any adjustments you might need, and your rights and entitlements.
Your options may include taking sick leave, reducing your hours, working from home, making changes to your role or duties, taking extended leave, or leaving work temporarily or permanently.
If you can't continue working, consider what income support you're entitled to, whether you can access your superannuation early, whether you have income protection insurance, and what other financial support is available.
Financial support
Cancer treatment can be expensive. Even with public healthcare, out-of-pocket costs for medications, appointments, parking, travel, and time away from work add up quickly. Financial worry adds significantly to overall stress.
There are government programs and community supports that can help reduce the financial burden.

Government assistance
You may be eligible for payments through Services Australia, such as:
- Sickness Allowance (for temporary inability to work)
- Disability Support Pension (for longer-term situations)
- Carer Payment or Carer Allowance (for family members caring for you)
Contact Services Australia (132 300) to discuss eligibility and application processes.
Other supports
- The Medicare Safety Net reduces out-of-pocket costs for medical services once you reach certain thresholds. Register your family at Medicare to track spending automatically.
- The Pharmaceutical Benefits Safety Net similarly reduces medication costs after you've spent a certain amount annually. Keep receipts from all PBS prescriptions to claim your safety net earlier.
- If you’re struggling with loan or credit payments, contact your bank early to discuss payment relief options
- In some cases, you may be able to access superannuation early on medical grounds. Speak to your fund, accountant or the Australian Taxation Office before applying.
A qualified financial planner can help you review your income, super, and insurance. You can find an accredited adviser through the Financial Planning Association of Australia.
Pancare also provides limited financial assistance for eligible patients and carers. Call 1300 881 698 or email support@pancare.org.au.
Legal considerations
It can feel confronting, but getting your legal documents in order gives peace of mind and helps your loved ones understand your wishes.
- A power of attorney is a legal document that lets someone you trust make decisions on your behalf if you become too unwell to do so. This can cover financial, legal, and personal matters, including health-care decisions.
- A Will sets out what happens to your property, finances, and personal items after your death. It can also include guardianship plans for children and your preferences for funeral arrangements.
- Estate planning means organising your assets, debts, and wishes ahead of time so everything is clear and simple for your loved ones.
- An advance care plan lets you record your preferences for future medical treatment. You can write these in an Advance Care Directive (sometimes called a “living will”), which only takes effect if you are unable to make or communicate decisions yourself.
Where to get help
Managing the practical side of cancer can feel overwhelming, but you don’t have to do it alone.
You can:
- Talk to a social worker or cancer care coordinator at your treatment centre
- Call Pancare Foundation on 1300 881 698 or visit pancare.org.au/living-well
- Contact the Cancer Council on 13 11 20 for advice on financial, legal, or work-related issues
Support and resources
You don't have to face oesophageal cancer alone. Many services and resources are available to support you and your family.
Pancare Support
Pancare Support is Pancare Foundation's dedicated support service for people affected by upper gastrointestinal (GI) cancers, like oesophageal cancer.
- Pancare Support Helpline is available Monday to Friday, 9am to 5pm. You can speak with a specialist upper GI nurse. You can book an appointment or alternatively call 1300 881 698.
- Pancare Support Groups are online or face-to-face support groups for people living withan upper GI cancer. You can share experiences with others who understand and learn from others' experiences.
- Carer Support Groups provide support for carers and family members. These are held online on the last Thursday of each month from 11am-12:30pm (AEST).
- Specialist Presenter-led Groups are monthly combined patient and carer groups that feature specialist presenters on topics like diet, managing side effects, and survivorship. These are held online on the third Thursday of each month from 11am-12:30pm (AEST).
- Financial assistance: Financial support is available for eligible patients, carers, and families. This can help with costs like medical equipment, bills, and specialist services.
- Educational resources: Pancare Foundation provides information booklets and guides, online resources, and a Living Well Series with expert information.

Cancer Council support groups
Cancer Council provides Australia-wide cancer information and support services, accessible regardless of cancer type.
The 13 11 20 Information and Support Line operates Monday to Friday, 9am-5pm, with trained consultants answering questions about cancer, treatment, services, and providing emotional support. Translation services are available for non-English speakers.
Telephone Support Groups run by Cancer Council NSW are free, professionally facilitated groups you can join from home. Contact Cancer Council on 1300 755 632 or email tsg@nswcc.org.au for information about joining these groups.
Face to face support groups are also available. Some groups are open to people with any type of cancer, while others are for people with a specific cancer type. Many support groups welcome family and carers.
Cancer Connect matches you one-on-one with someone who has experienced similar cancer. Speaking with someone who's been through oesophageal cancer treatment provides unique understanding and practical insights.
Legal and financial information through Cancer Council includes guidance on entitlements, managing costs, workplace rights, and legal issues. Their website offers downloadable resources and contact details for further assistance.
Your healthcare team
Your healthcare team is a key source of support. Don't hesitate to contact them with questions or concerns.
- Specialist cancer nurses provide information and education, help coordinate your care, offer emotional support, and are available for questions between appointments.
- Social workers can help with practical issues, connect you with financial support, provide emotional support and counselling, and help you navigate the healthcare system.
- Dietitians give specialist advice on nutrition, help with managing eating difficulties, provide advice on enzyme supplements, and offer ongoing nutritional support.
- Psychologists or counsellors provide support for emotional and mental health, teach strategies for coping, support you with anxiety and depression, and are available for you and your family.
- Exercise physiologists or physiotherapists design safe exercise programmes, help maintain strength and fitness, and support physical recovery.
- Pain specialists provide specialised pain management when pain is difficult to control.
- Palliative care teams help with symptom management and support for quality of life. They're available earlier than many people think - not just for end-of-life care. They can work alongside your cancer treatment team.
Online resources and information
Stick to reputable sources when looking for information online. Be wary of miracle cures or treatments that sound too good to be true.
Check when information was published as medical knowledge changes over time.
Discuss anything you read online with your healthcare team before making decisions.
Some reliable online sources include:
- Pancare Foundation (www.pancare.org.au) provides information about oesophageal cancer, support services, research and clinical trials, and resources and booklets.
- Cancer Council (www.cancer.org.au) offers information about all types of cancer, booklets and fact sheets, and videos and webinars. They also have Optimal Care Pathways available to show patients what they can expect from best practice cancer care.
- For clinical trials information, visit australiancancertrials.gov.au (Australian Cancer Clinical Trials) or gicancer.org.au (Australasian Gastro-Intestinal Clinical Trials Group).
How to find support services
The best place to start is with your healthcare team. They can refer you to appropriate services based on your needs.
You can also contact Pancare’s Support Helpline to speak with a specialist Upper GI Cancer Nurse.
- You can book a 45-minute appointment on Monday to Friday, 9am – 5pm (AEST/AEDT) for the cost of a local call.
- Alternatively you can call us on 1300 881 698 or simply send us an email pansupport@pancare.org.au
Want to talk?
Speak to an upper GI cancer nurse or counsellor, we're here to provide you with the support you need. Support available to anyone impacted by upper gastrointestinal (GI) cancer. Monday to Friday, 9am-5pm.
