Treating pancreatic cancer
There are several ways to treat pancreatic cancer, and your healthcare team will help you find the best plan for you. Your treatment will depend on things like where the cancer is, how much it has spread, your overall health, and what you want.
You'll be looked after by a team of specialists who are experts in treating pancreatic cancer. This section tells you about the different treatments available and what you can expect.
Treatment options for pancreatic cancer
Treatment goals
Treatment for pancreatic cancer depends on several factors, including the stage of your cancer, where it's located, your overall health, and your preferences.
Your doctor will explain what your treatment is aiming to do. In general, there are three different goals:

1. To cure the cancer
Some treatments aim to remove all the cancer and cure the disease. This often involves treatment with surgery, sometimes combined with chemotherapy.
Curative treatment works best when the cancer is found early and hasn’t spread.
2. To control the cancer and help you live longer
If the cancer can’t be removed with surgery, treatment can still slow its growth, ease symptoms and help you live well for longer. This may include chemotherapy, radiotherapy, or other treatments that keep the cancer under control.
3. To manage symptoms and improve comfort
When the cancer has progressed, the focus may shift to helping you feel as well as you can. This might involve pain relief, help with eating or digestion, and emotional or practical support.
Supportive (palliative) care can be given on its own or alongside cancer treatment.
Common treatments
Most people with pancreatic cancer will have a combination of treatments at different stages of their care. Your treatment team will explain what’s recommended for you and in what order.
Common treatments for pancreatic cancer include:
- Surgery can remove part or all of the pancreas and gives the best chance of cure when the cancer is found early. It’s often combined with chemotherapy before or after surgery.
- Chemotherapy uses medicines to destroy or slow the growth of cancer cells. It can be used before surgery (to shrink the tumour), after surgery (to reduce recurrence risk) or as the main treatment for advanced cancer.
- Radiation therapy (also called radiotherapy) uses targeted X-rays to destroy cancer cells. It’s less commonly used for pancreatic cancer, but can help reduce symptoms or prevent the cancer from returning.
- Targeted therapy: Some newer medicines target specific gene changes in cancer cells. If genetic or molecular testing shows your tumour has these changes, targeted therapy may be an option.
- Immunotherapy helps the body’s immune system find and attack cancer cells. At the moment, it’s available mainly through clinical trials for pancreatic cancer.
- Clinical trials test new treatments to see if they work better than current ones. Taking part in a trial can provide access to promising therapies and closer medical monitoring.
Your treatment team
Treatment for pancreatic cancer should be provided by a multidisciplinary team. This is a group of health professionals with different skills who work together to give you the best care.

Your main doctor
You should have one main doctor who coordinates your care. This is often:
- a medical oncologist (if chemotherapy is your main treatment)
- a surgeon (if surgery is planned)
- a gastroenterologist (if you're having tests to diagnose the cancer)
The multidisciplinary team
The rest of your multidisciplinary team will be made up of a mix of medical specialists, allied health professionals and supportive care professionals.
Each team member brings special skills to make sure all parts of your care are looked after. They meet regularly to talk about your case and agree on the best treatment approach.
The make-up of this multidisciplinary team may change at different stages of your treatment, but may include:
| Medical specialists | Allied health professionals | Supportive care professionals |
|
|
|
Making treatment decisions
Making choices about your treatment is an important part of your cancer journey.
You have the right to be involved in every decision about your care.
Your healthcare team is there to help you understand your options and support you to make choices that feel right for you.
Understanding your options
To make an informed decision, it helps to know as much as you can about your treatment choices. Your treatment team will explain:
- the different treatment options available to you
- the goals of each treatment (for example, cure, control, or symptom relief)
- the benefits and risks of each option
- possible side effects and how they might affect you
- what treatment involves — how long it takes, where it happens, and how often
- how it might affect your daily life
Things to think about
Everyone’s situation is different. When making treatment decisions, you might want to think about:
- your personal goals and what matters most to you
- your overall health and how fit you feel
- the side effects and how they could affect your quality of life
- practical issues such as travel, time off work, or caring for family
- your own values, beliefs and preferences
Questions to ask
It can help to write down your questions before appointments. You might like to ask:
- what treatment do you recommend, and why?
- what is the goal of this treatment?
- what are the benefits and possible risks?
- what side effects could I expect?
- how will treatment affect my everyday life?
- are there other treatment options?
- what happens if I choose not to have treatment?
- is there a clinical trial that might be suitable for me?
- how much will treatment cost?
- who should I contact if I have questions or feel unwell?
Taking your time
Although some treatments need to start quickly, you usually have time to:
- ask questions and get clear answers
- talk about your options with your family or friends
- ask for a second opinion if you want one
- think about what matters most to you before deciding.
Taking time to understand your options can help you feel more confident about your decisions.
Surgery for pancreatic cancer
Surgery gives the best chance of long-term survival for pancreatic cancer.
However, only a small number of people (around 15–20%) can have surgery when first diagnosed.
Your healthcare team will help decide if surgery is right for you.
The doctor in charge of your surgery is called a surgeon.
Will I have surgery?
You may be able to have surgery if the cancer is only in your pancreas or close by, and it hasn’t grown into major blood vessels. You also need to be well enough to manage a big operation.
Doctors use certain words to describe whether surgery is possible:
- Resectable (operable): The cancer can be removed with surgery.
- Borderline resectable: Surgery might be possible after chemotherapy to shrink the tumour.
- Locally advanced or metastatic: The cancer has spread too far, so surgery isn’t an option.
Types of surgery
The type of surgery depends on where the cancer is in your pancreas.
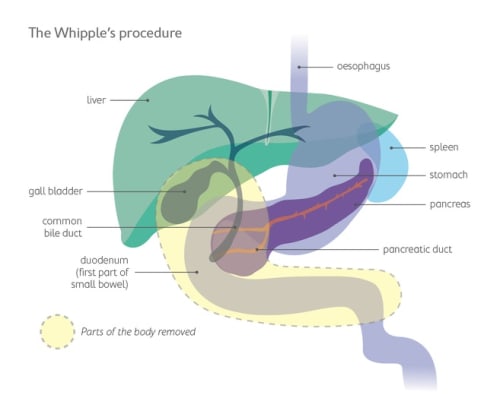
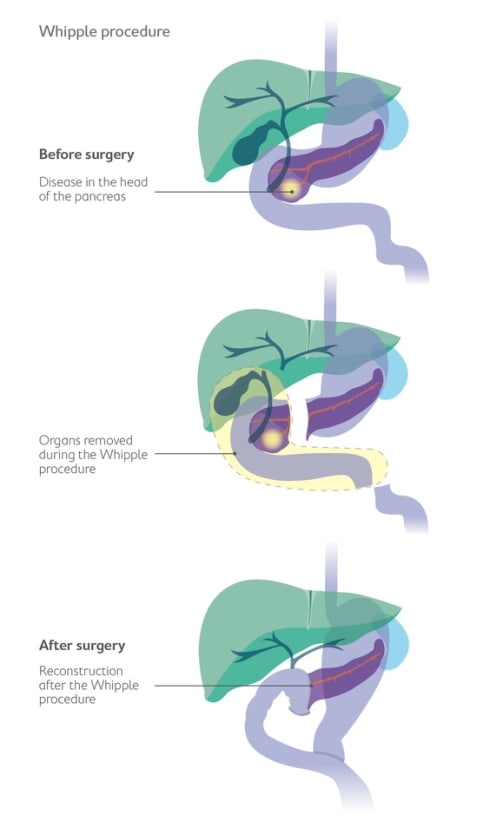
Whipple procedure (Pancreaticoduodenectomy)
This is the most common operation when the cancer is in the head of the pancreas.
The surgeon removes:
- the head of the pancreas
- the first part of the small intestine (duodenum)
- the gallbladder and part of the bile duct
- sometimes the bottom part of the stomach.
The remaining pancreas, bile duct and stomach are reconnected to the small intestine so your digestive system still works.
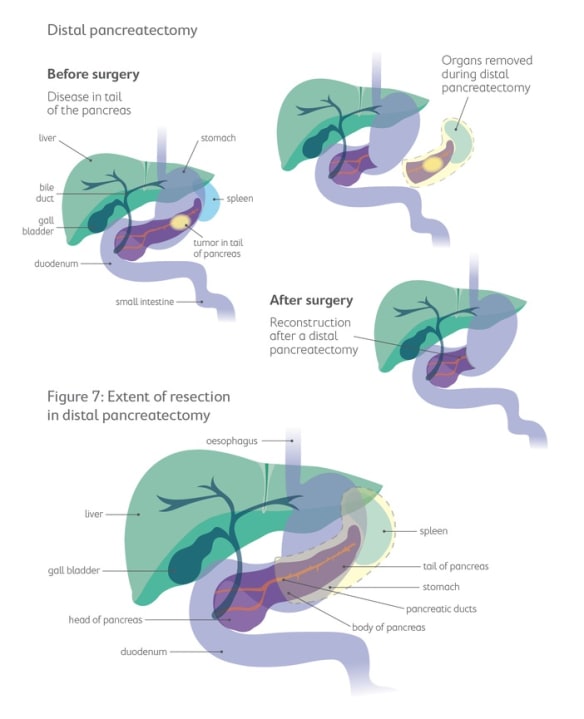
Distal pancreatectomy
This type of surgery is used when the cancer is in the body or tail of the pancreas.
The surgeon removes:
- the body and tail of the pancreas
- usually the spleen.
The head of the pancreas stays in place.
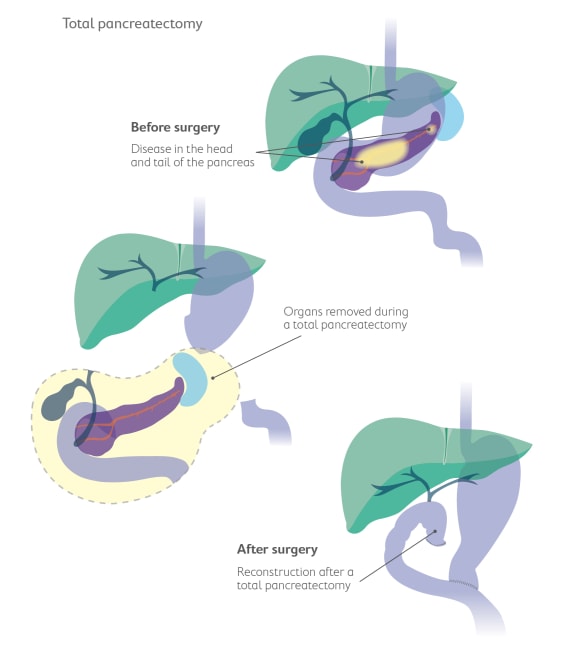
Total pancreatectomy
This operation removes the whole pancreas. It may also remove the gallbladder, part of the bile duct, parts of the stomach and small intestine, and often the spleen.
After this surgery, your body will no longer make insulin, so you’ll need insulin injections for life.
Bypass surgery
If the cancer can’t be removed, surgery may be done to ease symptoms.
This might include:
- creating a new path for food to pass from the stomach to the bowel
- creating a new path for bile to flow around a blockage.
Stent insertion
Instead of bypass surgery, a thin tube called a stent can be placed in a blocked bile duct to keep it open and relieve jaundice.
What to expect when having surgery
Before surgery
- You’ll have several tests to check you’re ready for the operation.
- You’ll meet your surgical team to talk about the benefits, risks and what recovery will look like.
During your hospital stay
- Most people stay in hospital for 1–2 weeks after surgery for pancreatic cancer.
- You may start your recovery in an intensive care or high-dependency unit.
- You’ll slowly begin to eat and drink again.
- Your team will help manage pain and watch for any problems.
Recovery at home
- Recovery can often take a few months. You’ll need some help at home, and it’s important to build up your strength slowly.
- Your care team will schedule follow-up appointments to check your progress.
- Surgery changes how your pancreas works. You might:
- Notice changes in digestion
- need pancreatic enzyme supplements (like Creon®)
- experience blood-sugar changes or diabetes
- notice appetite and weight changes.
Your healthcare team will help you manage these effects and adjust your diet if needed. A dietitian can support you with meal ideas and supplements.
Getting support
Having pancreatic surgery is a big step. It’s normal to feel anxious or tired.
You can ask for help from your care team, social worker or cancer support groups.
Pancare’s Support service can connect you with others who’ve been through surgery and recovery.

Chemotherapy for pancreatic cancer
Chemotherapy uses special medicines to kill cancer cells or stop them from growing.
It’s one of the main treatments for pancreatic cancer and can help people live longer and feel better.
The doctor in charge of your chemotherapy is called a Medical Oncologist.
Will I have chemotherapy?
Your oncologist may recommend chemotherapy:
- before surgery (called neoadjuvant therapy) to shrink the tumour and make surgery easier.
- after surgery (called adjuvant therapy) to lower the chance of the cancer coming back.
- as your main treatment when surgery isn’t possible.
Types of chemotherapy
Chemotherapy can be given in two main ways.
- Through a drip (IV chemotherapy). The medicine goes into a vein through a drip, usually in a hospital or cancer clinic. Each session can take a few hours, depending on your treatment plan.
- As tablets or capsules (oral chemotherapy). Some chemotherapy medicines come as tablets or capsules you take at home. Your oncologist will explain exactly when and how to take them.
What to expect during chemotherapy
Your chemotherapy plan
Your oncologist will design a plan based on:
- the stage of your cancer
- your overall health
- whether you’ve had surgery
- previous treatments
- clinical trials that might be suitable.
Most plans use a combination of drugs that work together to fight cancer cells.
Chemotherapy is usually given in cycles. This means you’ll have a period of treatment followed by a rest period so your body can recover.
A full course of chemotherapy often lasts several months. Your care team will explain the exact schedule for you.
Access devices
If you’re having IV chemotherapy through a drip, your doctor may recommend a device to make treatment easier. This might be:
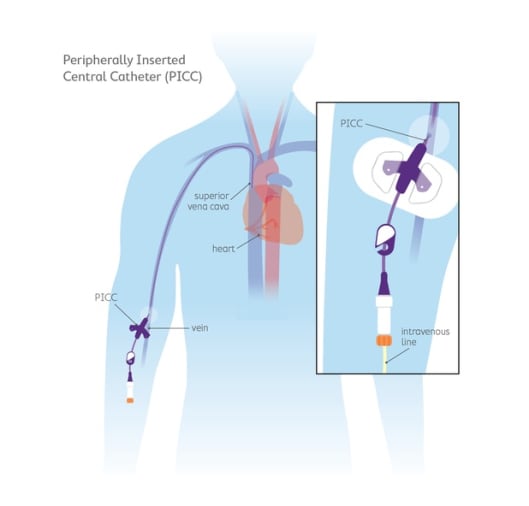
- a PICC line: a soft tube placed in a vein in your arm and threaded near your heart. It stays in during your treatment so you don’t need needles each time.
- a Port (Port-a-Cath): a small device placed under the skin of your chest that connects to a vein. It’s accessed with a special needle and can stay in for months.
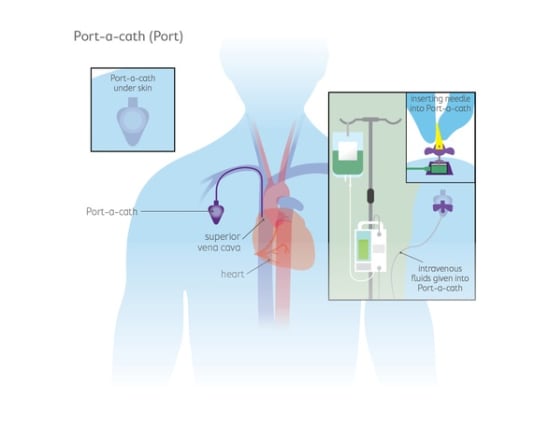
These devices help protect your veins and make treatment more comfortable.
Monitoring during treatment
You’ll have regular check-ups to make sure chemotherapy is working safely.
These may include:
- blood tests to check your blood counts and organ function
- scans to see how the cancer is responding
- check-ins to talk about how you’re feeling and any side effects
Side effects and how to manage them
Chemotherapy can affect healthy cells too, which causes side effects. Not everyone gets the same effects, and most can be managed well.
Common side effects include:
- feeling tired or weak
- feeling sick (nausea) or vomiting
- loss of appetite or changes in taste
- hair thinning or loss
- diarrhoea or constipation
- mouth sores
- numbness or tingling in your hands and feet
- higher risk of infections.
Your team can help by:
- prescribing anti-sickness or infection-preventing medicines
- adjusting your chemotherapy dose if needed
- providing nutrition and pain-management advice
- offering emotional and practical support.
Always tell your nurse or doctor about any side effects. There are often ways to make you feel more comfortable.
Getting support
Chemotherapy can be physically and emotionally tough. You don’t have to go through it alone.
Your care team, a dietitian, or Pancare’s Support service can help you manage side effects, plan meals, and find emotional support.

Radiotherapy for pancreatic cancer
Radiotherapy (also called radiation therapy) uses strong X-rays to destroy cancer cells.
It isn’t used as often as surgery or chemotherapy for pancreatic cancer, but for some people it can help shrink tumours, relieve symptoms, or improve comfort.
Will I have radiotherapy?
Your doctor may suggest radiotherapy:
- before surgery, alongside chemotherapy to shrink the tumour so surgery is easier.
- after surgery to treat any remaining cancer cells near where the tumour was removed.
- to slow down the growth of cancer that can’t be removed by surgery.
- to help ease pain or other symptoms in advanced pancreatic cancer.
How radiotherapy works
Radiotherapy targets cancer cells very precisely to reduce harm to healthy tissue around the pancreas.
Modern machines let doctors:
- aim radiation beams directly at the tumour
- protect nearby organs such as the stomach and bowel
- give small doses over several sessions to lower the risk of side effects.
You won’t see or feel the radiation, but it works inside your body to damage the DNA of cancer cells so they can’t keep growing.
Radiotherapy is often used together with a small dose of chemotherapy. This is called chemoradiation. The chemotherapy makes cancer cells more sensitive to radiation, helping the treatment work better.
Your oncologist will discuss whether this approach is suitable for you.

What to expect during radiotherapy
Before treatment
- You’ll have a planning session to prepare for radiotherapy.
- You might have a CT scan to help your team map out the exact treatment area.
- Small dots or tattoos may be placed on your skin so the radiation can be aimed accurately each time.
- Your team will explain how many treatments you’ll need and what to expect.
During treatment
- Treatment usually happens once a day, Monday to Friday.
- Each visit lasts about 15–30 minutes, but the radiation itself takes only a few minutes.
- You’ll lie still on a treatment bed while the machine moves around you.
- You won’t feel the radiation, and you’ll be able to go home afterwards.
- Most people have treatment for several weeks.
Side effects and how to manage them
Side effects usually appear slowly during treatment and improve a few weeks after it finishes. Everyone reacts differently, but common effects include:
- feeling tired
- skin redness or irritation in the treated area
- nausea or loss of appetite
- diarrhoea or softer bowel motions
- discomfort or a warm feeling in the abdomen
Your radiation oncology team will help you manage side effects. They can give advice about:
- gentle skin care
- anti-nausea or diarrhoea medicines
- eating well and maintaining energy
- when to contact your doctor if you’re worried.

Getting support
It’s normal to feel tired or emotional during treatment.
Your healthcare team can help with symptom control, nutrition, and emotional wellbeing.
You can also reach out to Pancare Support for practical advice, counselling, and connections with others living with pancreatic cancer.
Clinical trials
Clinical trials are research studies that test new treatments or new ways of using existing ones. They help doctors find better and safer ways to treat, diagnose, and manage pancreatic cancer.
For some people, joining a clinical trial can offer access to promising new treatments and specialised care before these options become widely available.
Why consider a clinical trial
Taking part in a clinical trial can give you the chance to try a new approach that may work better than standard care. You’ll be closely monitored by expert doctors and nurses who specialise in pancreatic cancer.
Even if the treatment being tested doesn’t benefit you directly, your participation helps researchers learn more about the disease and improve care for future patients. Many people find this sense of contributing to progress reassuring and empowering.

What kinds of trials exist
There are many different types of clinical trials.
Some test new chemotherapy drugs or combinations, while others explore targeted therapies that act on specific changes in cancer cells.
Researchers are also studying new ways to use immunotherapy to help the body’s own immune system fight cancer.
Other trials look at surgical techniques, how to better manage symptoms or side effects, or how to detect pancreatic cancer earlier.
Each trial has its own entry requirements, called eligibility criteria. These might include the type and stage of your cancer, your previous treatments, your general health, and sometimes genetic features found in your tumour.
Your healthcare team can explain which kinds of studies are currently running and whether one may be right for you.
Finding clinical trials
If you’d like to explore current pancreatic cancer trials, speak to your oncologist or visit trusted websites such as australiancancertrials.gov.au or the Australasian Gastro-Intestinal Trials Group.
You can also contact the Pancare Foundation for guidance and information about studies in Australia.
Complementary and alternative therapies
Many people with pancreatic cancer look for ways to feel better and support their wellbeing during treatment.
Complementary and alternative therapies are two types of approaches people sometimes use. It’s important to understand how they differ, and how they can safely fit into your care.
Understanding the difference
Complementary therapies are used alongside standard medical treatments such as chemotherapy, surgery or radiotherapy.
They aim to help you relax, manage symptoms, and improve your quality of life. Examples include meditation, yoga, massage, acupuncture, and relaxation techniques.
Alternative therapies, on the other hand, are used instead of standard medical treatments. These approaches have not been proven to treat cancer and can sometimes be harmful or interfere with your care.
For this reason, alternative therapies are not recommended as a replacement for evidence-based treatment.
Complementary therapies that may help
Some complementary therapies can be safely used to help with relaxation or symptom relief, as long as your healthcare team agrees.
- For relaxation and wellbeing: Gentle exercise, yoga, meditation, mindfulness, aromatherapy, massage (with your doctor’s approval), music therapy, and art therapy can help reduce stress and improve mood.
- For specific symptoms: Acupuncture and acupressure wristbands may help reduce nausea or pain. Some people find ginger tea or tablets helpful for nausea.
Simple breathing and relaxation exercises can ease anxiety and support sleep.

Dietary supplements
It’s common to wonder whether vitamins, minerals, or herbal products could help.
Some may be safe, but others can interfere with chemotherapy or other cancer treatments.
Always tell your healthcare team about any supplements you’re taking or thinking about taking. They can check for possible interactions and advise what’s safe.
Remember:
- High doses of some vitamins can be harmful.
- ‘Natural’ doesn’t always mean safe.
- Many products make claims that are not supported by science.
If in doubt, ask your doctor, pharmacist or dietitian before starting anything new.
Making informed choices
Before starting any new therapy, take time to check that it’s safe and worthwhile.
Talk to your healthcare team. They need to know everything you’re using. You can also ask:
- Is this safe to use with my cancer treatment?
- What are the possible risks or side effects?
- What evidence supports this therapy?
- How much will it cost and how often would I need it?
Follow-up care
After your initial treatment is complete, you'll enter a phase of follow-up care. This is an important part of your cancer journey.
Follow-up care involves:
- regular check-ups with your healthcare team
- watching for signs of cancer coming back
- managing ongoing side effects
- supporting your recovery and wellbeing
- coordinating care between specialists and your GP
Your follow-up care plan
Every person’s recovery is different. Your healthcare team will create a personalised follow-up plan that explains:
- Who your main contact person is (such as a nurse or specialist)
- How often you’ll need check-ups and who you’ll see
- Which tests you may need and how often they’ll be done
- What to expect at each visit
You may have blood tests (including tumour markers like CA 19-9), and CT or MRI scans from time to time to check for any changes.
These tests help your doctors see how you’re healing and detect any possible signs of the cancer returning early.
Managing ongoing issues
Some people continue to experience side effects after treatment, such as fatigue, digestive changes, or problems with appetite.
Your care team will support you to manage these issues and maintain your strength.
What to watch for
Your doctor will tell you about symptoms that may need to be checked quickly.
These might include:
- new or worsening pain in your tummy or back
- unexpected weight loss or loss of appetite
- jaundice (yellowing of your skin or eyes)
- ongoing tiredness that doesn’t improve with rest
- changes in your bowel habits
- new lumps, swelling or discomfort anywhere in your body
If you notice any of these symptoms, or anything that worries you, contact your healthcare team or GP as soon as possible.
Looking after yourself
Recovery takes time, both physically and emotionally. Keep communicating with your care team and let them know how you’re feeling.
Gentle physical activity, a balanced diet, rest, and emotional support from friends, family, or a counsellor can all make a big difference.
If you’d like extra support, Pancare Support can connect you with nurses, counsellors, dietitians and others who understand what you’re going through.
Want to talk?
Speak to an upper GI cancer nurse or counsellor, we're here to provide you with the support you need. Support available to anyone impacted by upper gastrointestinal (GI) cancer. Monday to Friday, 9am-5pm.
