Tests and diagnosis
You may need to have several tests when you are being investigated for stomach cancer. These tests help your healthcare team understand whether there are cancer cells in your stomach, what type of cancer it is, and whether it has spread to other parts of the body. This information is vital in planning the most effective treatment for you.
It can take time to complete all the necessary tests. Waiting for appointments and results can be stressful. But this process helps ensure your doctors have a clear and accurate understanding of your condition.
In this section, we explain the tests and investigations you might have, what staging means, how genetic testing may be used, and what to expect when you receive your diagnosis.

Tests for stomach cancer
If you doctor suspects that you have stomach cancer, you may need to undergo several different tests. Your doctor will choose the best tests for you. You may not need all the tests described here.
Physical examination
If you go to your doctor with symptoms like pain in your upper stomach, worsening reflux or difficulty swallowing, your doctor may perform a physical examination to check for signs of disease.
A physical examination is a check-up, where your doctor will look for things like lumps, swelling or anything else that seems unusual. They will ask you about your medical history, family history and your health habits.
Blood tests
Blood tests can check:
- your blood count
- how well your liver and kidneys are working
- tumour markers – chemical substances produced by cancers that show up in the bloodstream.
For example, CA19-9 and CEA are tumour markers linked to stomach cancer. But other health problems can also raise these markers, and some people with stomach cancer have normal levels. So, these tests alone can't tell you if you have stomach cancer.
Endoscopy and biopsy
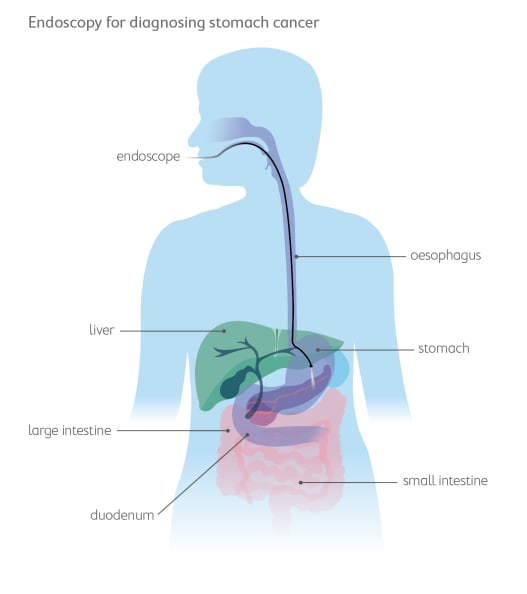
An endoscopy (also called gastroscopy) is the main test used to diagnose stomach cancer.
An endoscope is a thin, flexible tube with a small camera on the end. While you are sedated (asleep), the doctor will slide the endoscope down your oesophagus and into your stomach to look for abnormal areas.
The doctor will also take a small tissue sample during this procedure. This is called a biopsy. The biopsy is sent to a pathologist who looks at it under a microscope to check for signs of cancer.
Laparoscopy
A laparoscopy is a small operation done whilst you're asleep under general anaesthetic. A long tube with a camera is put in through small cuts in your tummy. This lets doctors see if cancer has spread. Small tissue samples (biopsies) can also be taken during this procedure.
Scans
Several types of scans may be used to look at your stomach and nearby organs.
- A Computed Tomography (CT) scan uses X-rays to make 3D pictures of your stomach and nearby organs. This scan usually also includes your chest and pelvis to check if cancer has spread.
- A Positron Emission Tomography (PET) scan uses a small amount of radioactive substance is put into a vein. It can help to find very small areas of cancer cells. You may have a PET scan combined with a CT scan.
- A Magnetic Resonance Imaging (MRI) scan uses magnets and radio waves to make detailed pictures of your stomach and the soft tissue nearby.
Waiting for test results
Results should be ready within two weeks of having the tests. Waiting can be stressful. If your symptoms get worse while waiting, contact your doctor or go to an emergency department if needed.
Even if you have been given an urgent referral, you may have to wait days or weeks for appointments and results. This is common. Any cancer growth during this waiting period is unlikely to cause additional harm if your symptoms are otherwise stable. However, it's still important to ask how long you may have to wait.
Genetic testing
Genetic testing can provide important information about both why a cancer develops and how it might best be treated.
While genetic testing in stomach cancer is not routine, there are two main types of genetic testing that you might hear about. One looks at the genes you were born with, and the other looks at the genes within the cancer itself.
Genetic testing for inherited gene changes
Sometimes, stomach cancer can run in families, but this is rare. Most people who get stomach cancer do not have a family link.
Genetic testing looks at your genes, which are like instructions inside your body that tell your cells how to grow and work. A small number of people may have a change (called a mutation) in one of their genes that increases their risk of stomach cancer.
If your doctor thinks your cancer might be linked to your family history, they may suggest genetic testing. This can help find out if other family members might also have a higher risk, and what steps can be taken to protect their health.
A genetic counsellor can explain what the test means for you and your family, and help you understand your options.

Genetic testing of tumours
If you are diagnosed with advanced cancer <Hyperlink to 6.0> in the stomach, oesophagus or gastro-oesophageal junction, your doctor may recommend a type of genetic test called molecular profiling.
Your doctor will send a sample of the tumour for testing in a laboratory, to see if there are certain molecules, proteins, or gene changes that can help decide which treatments are most likely to work for you.
For some people, this can include testing for:
- HER2. Some stomach cancers make too much of a protein called HER2. If your cancer is HER2-positive, you may benefit from medicines that specifically target this protein.
- PD-L1. This test helps doctors decide whether immunotherapy might be helpful.
- MSI-H or dMMR. These tests look for changes in the DNA repair system of the cancer cells. If the tumour has these features, certain immunotherapy drugs may work better.
These tests don’t change your diagnosis, but they help your team choose the most effective treatment for your type of stomach cancer.
Staging stomach cancer
Once stomach cancer is found, your doctors need to work out how far the cancer has spread. This is called staging.
Staging helps your medical team:
- understand how much cancer there is in your body
- plan the best treatment
- predict how you may respond to treatment.
In most cases, the stage of a cancer is based on three factors:
- the location and size of the tumour (T)
- whether or not the cancer has spread to nearby lymph nodes (N)
- whether or not the cancer has spread to distant areas of the body, known as metastasis (M).
These combined factors are known as the TNM staging system.
Your doctor might also use a number between 1 and 4 to describe the stage of your cancer.
- Stage 1: The earliest stage when cancer is found only in the lining of the stomach. Also called early stomach cancer.
- Stage 2: The cancer has spread deeper into the layers of the stomach wall.
- Stage 3: The cancer has spread to nearby lymph nodes. Also called locally advanced stomach cancer.
- Stage 4: The cancer has spread to other parts of the body (metastatic cancer) such as the liver, lungs, distant lymph nodes or to the tissue lining the abdominal cavity (peritoneum). Also called advanced or metastatic stomach cancer.
Finding out you have stomach cancer
Being told you have stomach cancer is shocking and overwhelming. There is no ‘right’ way to feel – everyone reacts differently. You may feel:
- shock and disbelief
- fear and worry
- anger
- sadness
- fear and uncertainty for the future

All of these reactions are normal.
A lot can happen quickly after diagnosis, and you might get lots of information. It's okay if you don't remember everything you're told or need information repeated.
What happens next
After your diagnosis, your medical team will finish any remaining tests that are needed. They will then talk to you about the treatment plan best suited to your situation.
Treatment should start within four weeks of diagnosis, depending on how urgent it is and what type of treatment is recommended.
Here are some questions that you may want to ask your medical team as you come to terms with your diagnosis and think about your treatment options.
- What type of stomach cancer do I have?
- Where in the stomach is the cancer located?
- Has the cancer spread, and what stage is it?
- How does this stage affect my treatment options and outlook?
- What treatments are recommended for my situation?
- Can I get a second opinion?
- What is the goal of treatment? Is it to remove the cancer, slow its growth, or manage symptoms?
- What are the benefits and risks of each option?
- How likely is the treatment to work in my case?
- Are there other treatments I should consider (including clinical trials)?
- What happens if I decide not to have treatment?
Want to talk?
Speak to an upper GI cancer nurse or counsellor, we're here to provide you with the support you need. Support available to anyone impacted by upper gastrointestinal (GI) cancer. Monday to Friday, 9am-5pm.
