Pancreatic cancer pathways
Pain management and palliative care
Content developed in collaboration by University of Melbourne, Faculty of Medicine, Dentistry and Health Sciences
Overview
Pain and symptom management are critical components of supportive care for people with pancreatic cancer. These clinical resources are designed to assist health care practitioners in facilitating timely access to specialist pain management and palliative care. They offer practical, evidence-based pathways for referral, including tools for assessing pain needs, clinical guidance to support early integration of palliative care and culturally sensitive care. This empowers clinicians to make informed decisions and support patients effectively throughout their care journey.
Pain management pathway
Full document available here
Purpose of this Clinical Guidance Section
This section aims to support health care practitioners to screen and assess pancreatic cancer patients for pain. It focuses on:
- Pain screening and initial assessment for people with pancreatic cancer
- Comprehensive pain assessment for people with pancreatic cancer
- Access to timely pain management for people with pancreatic cancer
- Interventional pain management for people with pancreatic cancer
- Radiotherapy in the management of pain in people with pancreatic cancer
- Clinical guidance for access to assessment and timely pain management for Aboriginal and Torres Strait Islander People
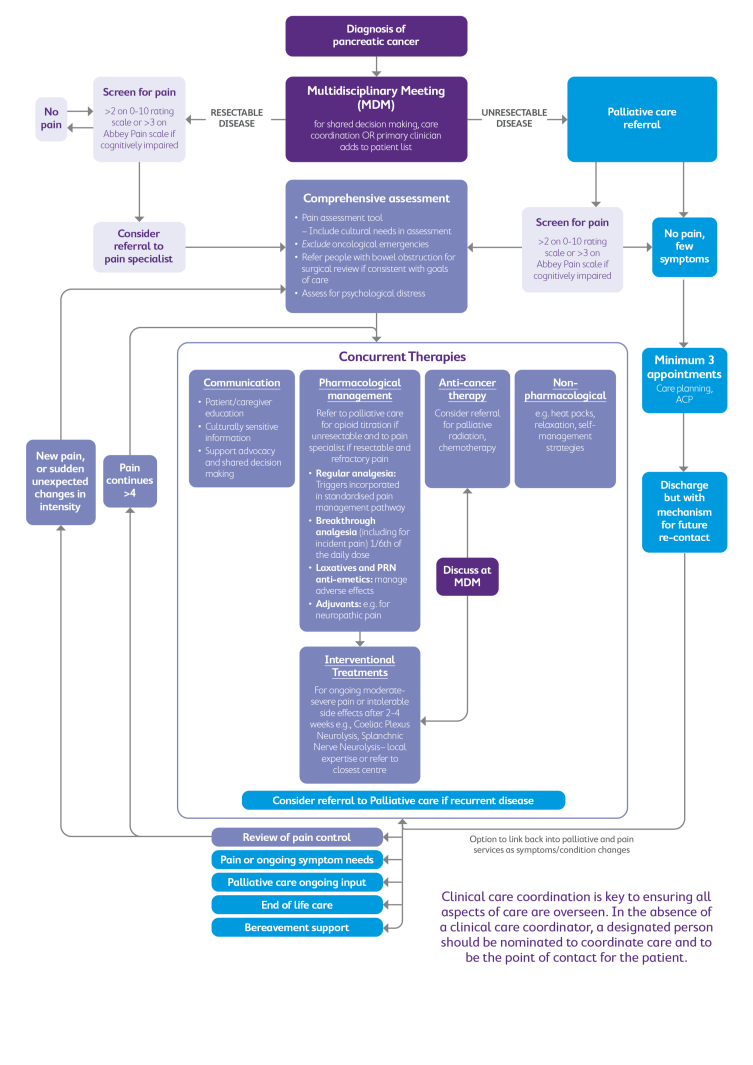
Pathway to rapid access pain management for people with pancreatic cancer
You can view and download the interactive version of this diagram below here.

Click below to discover more
A patient information brochure: Interventional pain management in pancreatic cancer is available to read, download and print. For an eBook version of the patient information brochure, please click here.
A postcard is available to read, download and print for patients here.

Clinical Recommendations
1. Pain screening and initial assessment for people with pancreatic cancer
Pain screening and initial assessment for people with pancreatic cancer should occur at every clinical encounter using a 0–10 scale. If pain is present, follow-up questions explore abdominal and back pain, night pain, positional discomfort, and treatment side effects to guide timely referral and management. Click here for the Pancreatic Cancer Pain Assessment Tool. Click here for Clinical Guidance and Principles of Pain Screening and Initial Assessment.
2. Comprehensive pain assessment for people with pancreatic cancer
Comprehensive pain assessment for people with pancreatic cancer is required when pain is reported or changes occur. It includes evaluating pain severity, location, timing, interference, and specific symptoms (abdominal discomfort, back pain, night pain, positional discomfort). Additional factors such as disease status, cultural beliefs, psychosocial distress, current management, and patient preferences are assessed to guide tailored pain management and timely referral. Click here for Clinical Guidance and Principles of Comprehensive Pain Assessment for People with Pancreatic Cancer.
3. Access to timely pain management for people with pancreatic cancer
Timely pain management for people with pancreatic cancer relies on early identification and rapid referral to specialist pain and/or palliative care services. Multidisciplinary team meetings help flag patients with complex pain needs, while barriers such as opioid stigma and misconceptions about palliative care must be addressed through clear communication. Telehealth and care coordination improve access for rural and regional patients, ensuring equitable, patient-centred pain relief across the illness trajectory. Click here for Clinical Guidance and Principles of Access to Timely Pain Management for People with Pancreatic Cancer.
4. Interventional pain management for people with pancreatic cancer
For patients with pancreatic cancer and refractory pain, interventional options such as coeliac plexus or splanchnic nerve neurolysis can provide significant relief and reduce opioid use. Early referral to pain or palliative care specialists is recommended, with procedures performed by interventional radiologists, gastroenterologists, or pain specialists. Other advanced options include intrathecal analgesia for severe, unresponsive pain. These interventions require multidisciplinary planning, clear communication, and consideration of patient preferences and clinical risks. Click here for Clinical Guidance and Principles of Interventional Pain Management for People with Pancreatic Cancer.
5. Radiotherapy in the management of pain in people with pancreatic cancer
Radiotherapy can help relieve pain in pancreatic cancer when analgesics are insufficient. Hypofractionated courses and stereotactic body radiotherapy have shown benefits, with up to half of patients achieving complete pain resolution and reduced analgesic use. Referral to a radiation oncologist should be considered for uncontrolled pain, with multidisciplinary planning and awareness of potential gastrointestinal side effects. Click here for Clinical Guidance and Principles of Radiotherapy in the Management of Pain in People with Pancreatic Cancer.
6. Clinical guidance for access to assessment and timely pain management for Aboriginal and Torres Strait Islander People
Effective pain assessment in pancreatic cancer requires listening carefully, building trust, and using clear, culturally appropriate language. For Aboriginal and Torres Strait Islander patients, pain may be described differently (e.g., “okay pain,” “no good pain”), and holistic assessment should include physical, emotional, and spiritual aspects. Early involvement of Aboriginal health workers, clear explanations of medications, and addressing opioid stigma are essential to ensure timely, equitable pain management. Click here for Things Health Professionals should know for Optimal Pain Assessments for People with Pancreatic Cancer Clinical guidance for access to assessment and timely pain management for Aboriginal and Torres Strait Islander People.
Palliative care pathway
Full document available here
Purpose of this Clinical Guidance Section
This section aims to support health care practitioners to screen and assess pancreatic cancer patients for pain. It focuses on:
- Access to early palliative care for people with pancreatic cancer
- Clinical guidance for access to early palliative care for Aboriginal and Torres Strait Islander People
Integrated pathway to rapid access pain management and early palliative care for people with pancreatic cancer
You can view and download the interactive version of this diagram below here.
Clinical Recommendations
1. Access to early palliative care for people with pancreatic cancer
Early palliative care should be introduced soon after diagnosis of metastatic or unresectable pancreatic cancer, alongside active treatment. It improves quality of life, symptom control, and reduces unnecessary hospitalisation, with evidence showing benefits for patients and families when integrated early rather than late. Click here for Clinical Guidance and Principles of Access to Early Palliative Care for People with Pancreatic Cancer.
Multidisciplinary Meetings
Multidisciplinary Cancer Meetings (MDMs) provide a collaborative forum for discussing pancreatic cancer cases, enabling shared decision-making, care coordination, and timely identification of patients who may benefit from specialist pain management or early palliative care. These meetings ensure that therapeutic dilemmas are addressed and that patients with unresectable or metastatic disease are promptly referred for supportive care
For Referrers
Referrers should initiate early palliative care for patients with metastatic, unresectable, or otherwise inoperable pancreatic cancer, recognising its role in managing pain, psychological distress, and existential concerns. Effective referral involves normalising palliative care as part of high-quality treatment, clearly explaining its supportive functions, and ensuring timely access through outpatient, community, or telehealth services depending on patient needs and local availability.
For Palliative Care
Palliative care consultations for people with pancreatic cancer should include comprehensive assessment of pain, psychological distress, spiritual concerns, and family needs, while supporting advance care planning and home-based supports. Early palliative care differs by focusing on communication, rapport-building, and future planning, especially for patients with fewer symptoms, and should be delivered alongside usual cancer treatments. Early palliative care may be a time-limited intervention (a minimum of three consultations), with clear pathways for follow-up or re-referral.
Telehealth
Telehealth is a valuable option for delivering early palliative care to people with pancreatic cancer, especially in areas lacking outpatient services. It enables access to specialist support, reduces travel and hospital burden, and is considered acceptable and effective by both patients and clinicians, despite not fully replacing face-to-face care.
2. Clinical guidance for access to early palliative care for Aboriginal and Torres Strait Islander People
Best palliative care for pancreatic cancer requires listening, trust, and culturally safe practice. For Aboriginal and Torres Strait Islander people, care should respect self-determination, family involvement, and holistic views of health (physical, emotional, spiritual). Early engagement with Aboriginal health workers, clear communication, and continuity of care are essential to reduce distress and ensure equitable, person-centred support. Click here for Things Health Professionals should know for Best Care in Palliative Care for People with Pancreatic Cancer Clinical guidance for access to early palliative care for Aboriginal and Torres Strait Islander People.
Education module
More detailed learning on pain and palliative care can be found in the online module, click here to start learning.




